
INTRODUCTION
Yesterday I was sitting at a cafe. On my left table were two young moms, each with a child on the spectrum. Both of them were concerned about the challenges the children faced, in general. Politely and promptly I introduced myself and started discussing it.
One of them expressed, “Just imagine my child who is quite charming, bright, and imaginative- yet resists even the simplest of everyday demands with anxiousness, meltdowns, or complete shutdowns. Sometimes it is difficult for me to handle.”
What do you think this is? It is not stubbornness or bad behavior. For many autistic children with Pathological Demand Avoidance (PDA), this is their reality.
Let us dive into this article and let us empower these children while shifting from control to connection.
What is Pathological Demand Avoidance (PDA)?
Pathological Demand Avoidance (PDA) was coined by Elizabeth Newson in the 1980s.
The term was used to describe the children within the autism spectrum who showcase obsessive resistance to everyday demands and requests.
Those on the spectrum are said to:
- So in a broader aspect, PDA sounds like the way we already describe those on the spectrum. So, why do we need yet another diagnosis that sets the child up for negativity?
- According to Rachna Sahney Pargi , the diagnosis of PDA will help the parents, teachers, caregivers or therapists of the autistic individuals to understand and find new ways to support them and help them live their best lives.
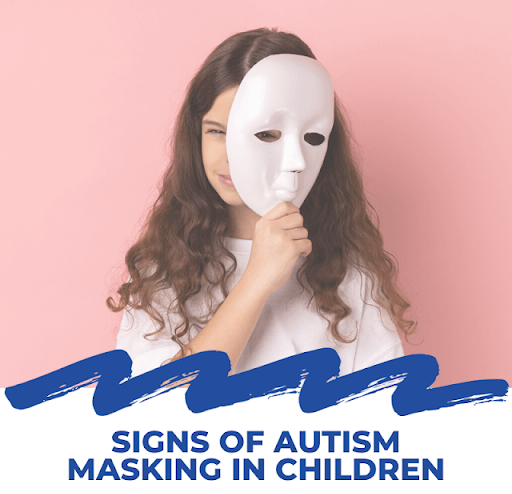
- Individuals with PDA exhibit behaviors driven by high anxiety, need for control, avoiding demands through strategies like negotiation, distraction, and so on. An interesting take, otherwise is that PDA individuals may appear sociable on the surface but struggle with emotions.

Understanding the PDA Profile
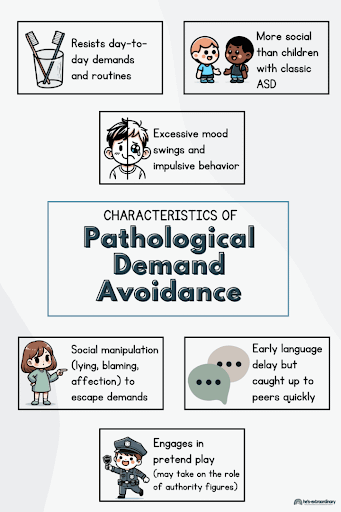
There are set of challenges, and the key features include:
- Social manipulation: Resisting daily demands or routine activities by tactful and extreme lengths to avoid and control the situation is quite common.
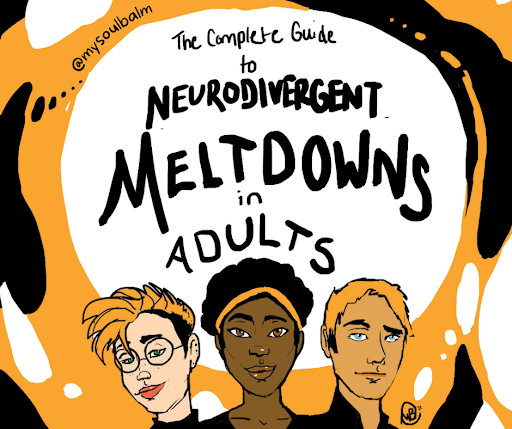
- Emotional dysregulation: The disorders like stress and anxiety are quite common amongst the autistic individuals.
- Obsessive behavior: Often these individuals come out as defiant or oppositional or stubborn. But the underlying cause is often anxiety rather than intentional misbehavior.
- Language delay due to passivity
- Role playing and pretending: Use of distractive techniques or role playing to dismiss expectations is used. It can be extreme in nature and end up sinking to panic attacks or meltdowns if the demands are enforced on them.
- Surface sociability: Appearing socially adept yet struggling with deeper social understanding and interactions.
Does a PDA Diagnosis Support or Separate?
The “Can’t” VS “Won’t” Dilemma
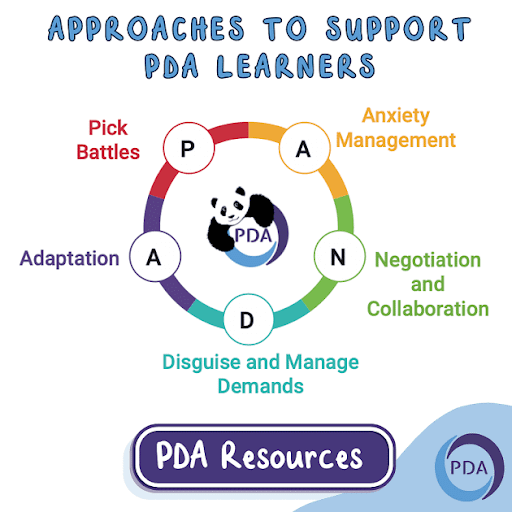
Supporting Children with PDA: Strategies and Approaches
There are set of challenges, and the key features include:
Understanding the Child’s Experience
- Notice signs of anxiety: Avoidance or withdrawing, skin picking, fidgeting or repetitive actions, anger/ laughing/ crying, restlessness, masking, obsessing, running off or hiding, remaining silent.
- Spot difficulties with understanding and using language: Some individuals may have expressive language but cannot process verbal communications promptly. Give them time to interpret and process effectively.
- Recognize struggles with social interaction: An individual with autism may not understand the “unwritten rules” used in social interactions. They might invade personal spaces or be close while talking or might not catch on to a person’s voice and tone or the body language they use.
- Be aware of emotional confusion: May feel overwhelmed, unable to understand or unable to “label” their emotions effectively.
- Identify when they feel unsure or overwhelmed: Just know what things “zone them out”, what might be expected of them, when a problem might end, and whether they can cope with whatever may come.
- Notice signs of sensory overload: Elevated sensory perception can lead to anxiety, overload, and so on.
How Parents and Caregivers Can Adapt
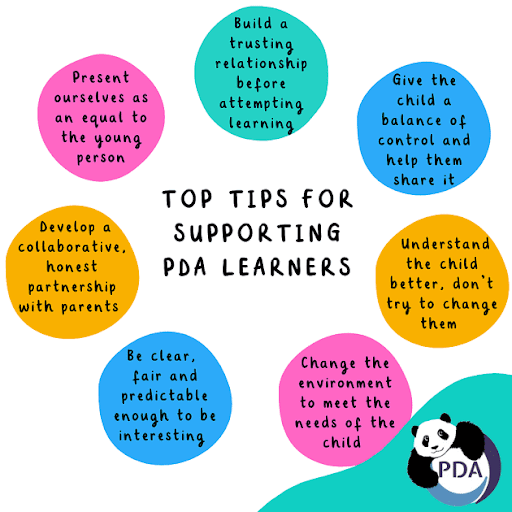
- Shift your perspective to better support them: Look beyond surface behaviors for a deeper reason, do not take things personally
- Change the environment to make things easier: Right environment includes consistent boundaries, rewards, consequences, praise, and approach using negotiation, collaboration, and flexibility.
- Find the right balance between flexibility and structure: The ability to cpe up will vary on a daily basis, so control the “input” of demands. And make sure to incorporate “recharge time” to allow anxiety to lessen and tolerance level to grade up.
- Give them extra time when needed: Allow them time to settle and make sure to add extra time. For instance, setting alarms earlier on school mornings. Allow flexibility!
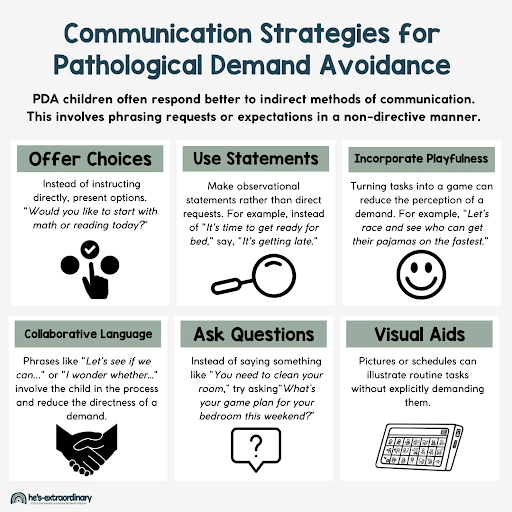
- Lower the pressure they may feel from requests: Change the tone, phrase, and language. For example, use “Your night suit is on bed, I am here if you need any help,” rather than “You are supposed to get dressed for bed now.”
- Speak in less direct ways when helpful: Indirect communication includes physical prompts like you can tap or spot on the night suit instead of saying,”Please put your night suit on” or visually impart the information. One can use sticky notes or communicate via pictures.
- Use distractions or turn tasks into playful activities: Do not demand. For instance, “Let us see who can name all the colors of each piece of clothing” when getting dressed.”
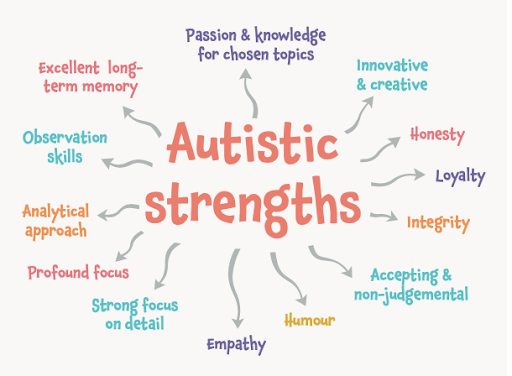
- Lighten the mood with humor: Humor is a great way to make them feel relaxed and lessen the perception of demands.
- Ask for help: Ask your child to help you with something you “cannot recall” or “do not know.” You can demand in an indirect way.
- Let them make choices where possible: Offer choices so that they can choose between them. For instance, you might ask, “Would you like to have a bath at 7:00 or 8:00 tonight?”
- Help meet their sensory comfort needs: Provide sensory comforts and that also depends on the anxiety levels, surroundings and so on. Headphones (to eliminate unwanted noise), Chewy toys (for oral sensory input), Scented objects (candle, soap or perfume to avoid unwanted smells), Sun or tinted glasses (for oversensitivity to light)
Encouraging Communication and Connection
- Give them more time to respond: This will offer them time to process, respond and interact effectively. After a statement, count to five (can vary) slowly in your head.
- Be clear and simple, but not too direct: Break down your requests or questions in smaller parts.
- Practice through pretend play or acting out situations: For instance, state, “I am not able to recall where the blue cups are. Can you help me put them on the plates?”
- Use stories, shows, or games to teach social skills: These can help children learn about emotions, relationships, and understand social dynamics.
CONCLUSION
“For the minds that seek, not settle.” —
Written by Dr. Sakshi- May, 2025.
WHAT'S NEXT FOR YOU?
Stay tuned with Rachna Sahney Pargi for more articles that dive deep into human diversity, mental health, and how to navigate life in a neurodiverse world.
Reference
- O’Nions E, Gould J, Christie P, Gillberg C, Viding E, Happé F. Identifying features of ‘pathological demand avoidance’ using the Diagnostic Interview for Social and Communication Disorders (DISCO). Eur Child Adolesc Psychiatry. 2016;25(4):407-419. doi:10.1007/s00787-015-0740-2
- Milton D. E. (2013). ‘Nature’s answer to over-conformity’: Deconstructing pathological demand avoidance. Autism Experts. https://kar.kent.ac.uk/62694/
- Kildahl, A. N., Helverschou, S. B., Rysstad, A. L., Wigaard, E., Hellerud, J. M., Ludvigsen, L. B., & Howlin, P. (2021). Pathological demand avoidance in children and adolescents: A systematic review. Autism, 25(8), 2162-2176. https://doi.org/10.1177/13623613211034382 (Original work published 2021)
- NewsonE, Le Marechal K, David C. Pathological demand avoidance syndrome: a necessary distinction within the pervasive developmental disorders. Arch Dis Child. 2003;88:595–600. doi: 10.1136/adc.88.7.595. [DOI] [PMC free article] [PubMed]
- O’Nions E, Viding E, Greven CU, Ronald A, Happé F. Pathological demand avoidance (PDA): exploring the behavioural profile. Autism: Int J Res Pract. 2013;8:538–544. doi: 10.1177/1362361313481861. [DOI] [PubMed]

No comments yet. Be the first!