Introduction
“A stitch in time saves nine.”
When it comes to understanding your child’s developmental milestones, this old proverb couldn’t ring truer.
Recognising the early signs of autism and getting a diagnosis can make all the difference in your child’s journey. Autism is not something that comes with a user manual. It is a neurological condition that affects the child’s communication, ability to interact socially, and process information. But one thing is clear– early intervention works wonders. So, now you must be pondering– how do you test a child for autism, where do you ever begin?
This blog will navigate the process with confidence and compassion.
Trust your Parental Instincts and look for Early signs.
There is a reason people say, “Mother knows the best.”
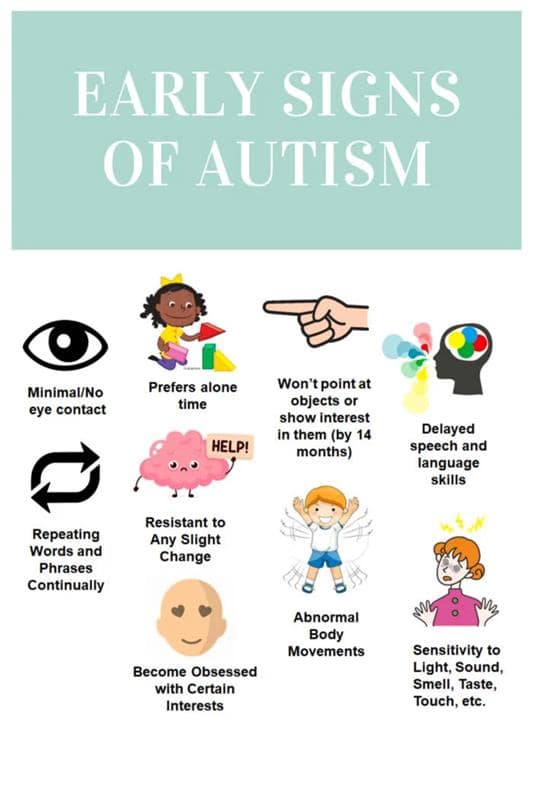
Parents are often the first to notice something that is indifferent or unique in their child’s behavior. Maybe your toddler avoids eye contact, does not respond to their name, or lines up toys instead of playing with them. These may seem like quirks, but when they persist, they could be early signs of autism.
The American Academy of Pediatrics suggests that autism- specific screening should be at 18 and 24 months of age.
Common early signs of Autism—
- Behavior
2. Communication
3. Cognition
If your gut is telling you something, do not brush it off. Begin by taking notes of your child’s behavior or any developmental delay you notice.
Talk to your Doctor first
“A journey of a thousand miles begins with a single step.” Consult a healthcare professional or an individual who is relevant to this. Bring your observations to their attention and understand that no concern is too small.
A developmental screening for autism will be conducted. A short test to see if your child is learning basic skills when they should.
Developmental Screening Tools:
- M-CHAT-R/F (Modified Checklist for Autism in Toddlers): A widely-used screening tool for toddlers between 16 and 30 months.
- Ages and Stages Questionnaire (ASQ)
- CDC’s Developmental Milestones Checklists
Understand that these screenings are not diagnostic. They are a way to flag potential concerns. If the results raise red flags, the next step is a comprehensive evaluation.
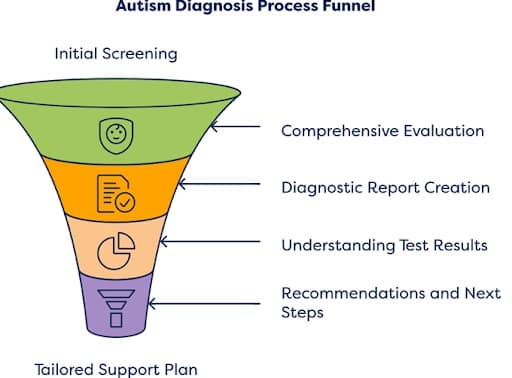
Comprehensive Autism Evaluation
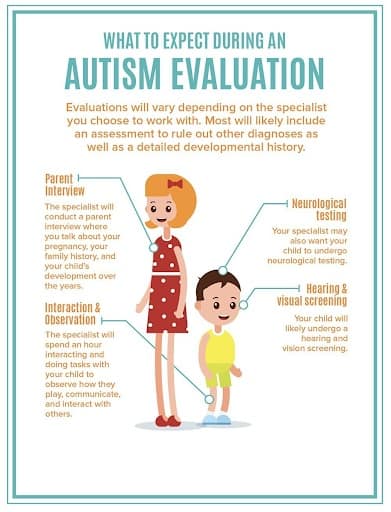
This is a part where things get more formal, thorough, and detailed. If your child shows signs of autism in the initial screening, your doctor will refer you to a specialist.
Who Can Diagnose Autism?
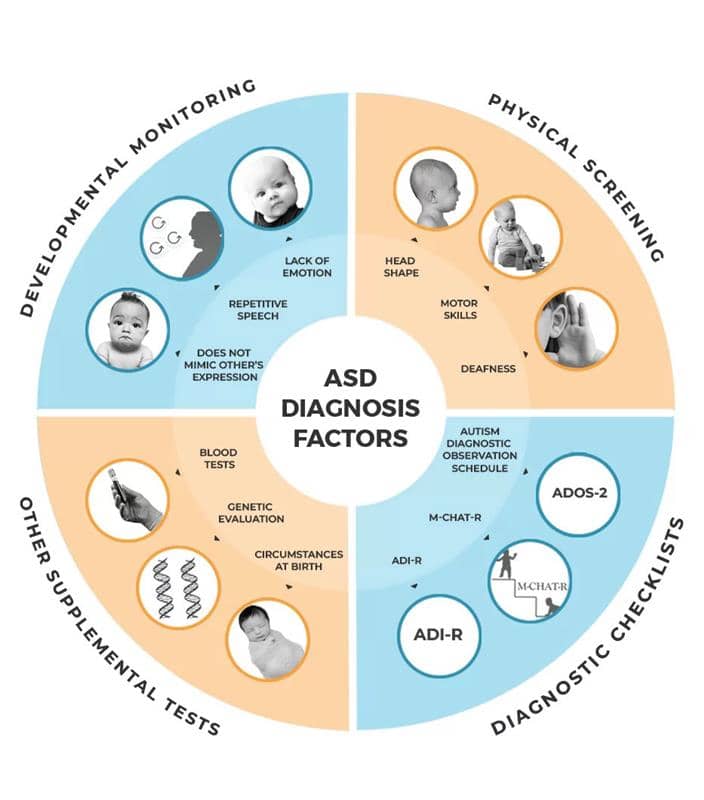
These professionals will use standardized diagnostic tools like:
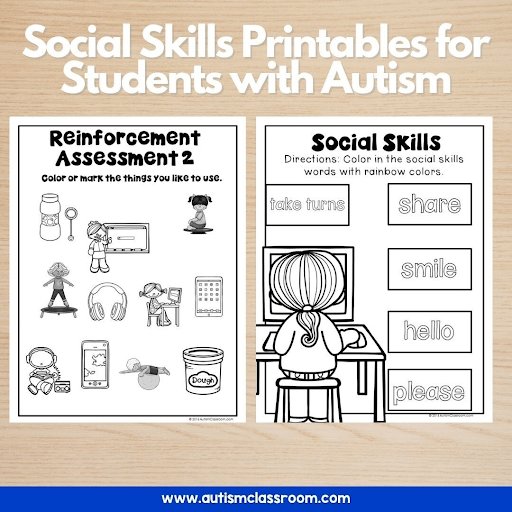
They will assess communication skills, social interaction, play, behavior, and sensory processing through interviews, questionnaires, and play-based assessments.
What to Expect:
Understanding the Diagnosis
After the evaluation, the specialist will share whether your child meets the criteria for autism according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
The DSM-5 looks for:
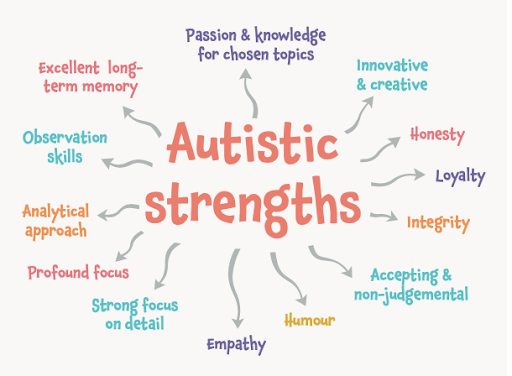
Do not panic at all if you hear the words “on the spectrum.” Autism is not just that– a spectrum. It is beyond that. Some children might need significant aid, while others might grow up needing minimal assistance.
In fact, early diagnosis (as young as 18 months) allows for interventions that can greatly improve long-term outcomes in communication, behavior, and learning.
After the diagnosis- What’s next?
This is often the most emotional part for parents. It is fine to feel overwhelmed. Recall, “Every cloud has a silver lining.” A diagnosis is not an end- it is the beginning of understanding your child better.
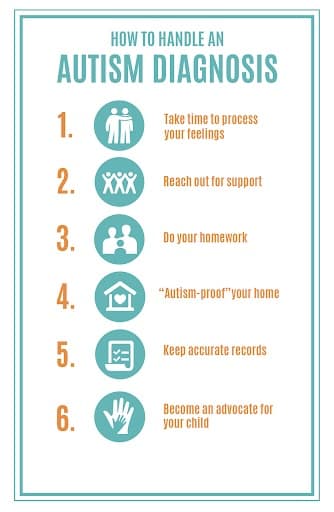
Steps to take:
Aid your child with the tools they need to thrive– and that starts with timely therapy and consistent routines.

Can Autism be misdiagnosed?
Yes, and that’s why it’s crucial to work with trained specialists. Some children might be misdiagnosed with:
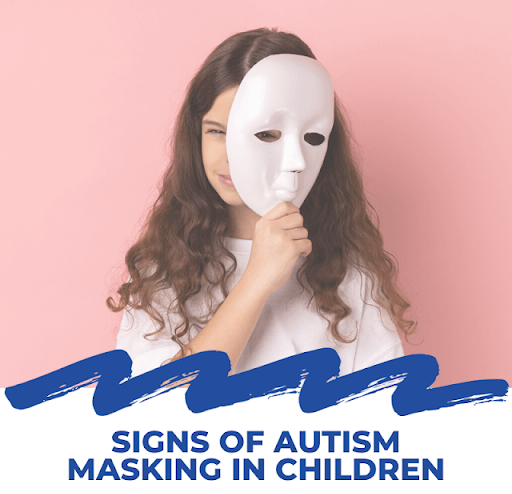
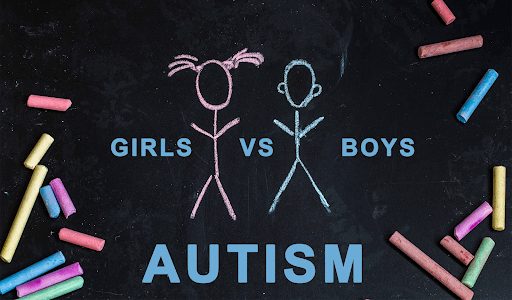
Others might go undiagnosed, especially girls who often display symptoms differently. Girls with autism may mask their behaviors, making it harder to spot. In fact autism is four times more common in boys than girls, but girls are often diagnosed later.

Empowering yourself with Knowledge and Support
You are definitely not alone. There is an entire community of parents walking on the same road.
Helpful resources:
- Autism speaks– toolkits and local resources
- CDC’s learn the signs. Act Early.
- Rachna Autism Care
- National Autism Association
- Local Parent support groups and social media communities
Join the webinars, attend workshops, and keep asking questions. The more you know, the more you can help your child.
Conclusion
A diagnosis doesn’t change who your child is. It simply gives you a roadmap to guide them better. Celebrate their uniqueness. Cherish their wins, big or small.
Because at the end of the day, “The child who is not embraced by the village will burn it down to feel its warmth.” Let your child know they are seen, heard, and supported.
Here’s What You Can Do Today:
- Observe your child’s behavior
- Talk to your pediatrician
- Don’t wait—book a screening
- Seek support and information
You’re not looking for labels. You’re looking for answers—and support. And that’s what testing for autism is all about.
What’s Next For You?
Want to learn more about embracing your unique brain? Stay tuned Rachna Sahney Pargi Journey for Autistic Child Support, for more articles that dive deep into human diversity, mental health, and how to navigate life in a neurodiverse world.
Reference
- Ghaneshirazi, Zahra. (2018). Autism Spectrum Disorder. (PDF) Autism Spectrum Disorder
- Hodges H, Fealko C, Soares N. Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation. Transl Pediatr. 2020;9(Suppl 1):S55-S65. doi:10.21037/tp.2019.09.09
- Naji, Wafaa & Qasim Waheeb, Mohammed. (2020). Autism Spectrum Disorder: Review Article. Medico-Legal Update. 20. 324-329. (PDF) Autism Spectrum Disorder: Review Article
- Wikipedia. (n.d.). Autistic Masking. Retrieved from [https://en.wikipedia.org/wiki/Autistic_masking]
- Adams, J. B., Johansen, L. J., Powell, L. D., Quig, D., & Rubin, R. A. (2011).Gastrointestinal flora and gastrointestinal status in children with autism – comparisons to typical children and correlation with autism severity. BMC Gastroenterology,11(1). doi:10.1186/1471-230x-11-22


No comments yet. Be the first!